10 Medical Misconceptions Doctors Wish You Should Stop Believing
The internet is a powerful tool, but unlike your new phone or kitchen gadget, it doesn’t come with a user manual. You can look up anything—from how to bake bread without yeast to ancient surgical techniques—but knowing what to believe is a different story altogether.
Since the rise of social media—and even more so during the COVID-19 pandemic—we’ve seen a tidal wave of medical misinformation sweep across the web. Ideas that sound scientific can gain traction simply because they go viral, not because they’re true. And that’s where things get dangerous.
From miracle cures to conspiracy theories, these misleading claims don’t just confuse people—they can actively put lives at risk. That’s why it’s more important than ever to learn how to separate fact from fiction when it comes to your health. The right knowledge can be life-saving; the wrong one… well, not so much.
10. Why 70% Rubbing Alcohol Works Better Than 90%—And It’s Not What You Think

Back when the pandemic began and shelves were stripped clean of disinfectants, one odd thing stood out: while 90% or even 99% rubbing alcohol vanished fast, you could still find bottles of 70% alcohol collecting dust. Most people assumed the higher the percentage, the stronger the germ-killing power. Makes sense, right?
Well… not quite.
In a twist of counterintuitive science, it’s actually 70% alcohol that wins the sanitizing game for most surfaces. Why? Because that 30% water content plays a crucial role. It allows the solution to spread more effectively, linger on surfaces longer, and actually break down the cell walls of bacteria and viruses before evaporating. A higher alcohol concentration evaporates too quickly—often before it can do the job properly.
Think of it this way: if the alcohol vanishes in seconds, it doesn’t get the chance to neutralize the pathogens. That lingering water helps carry the alcohol deep into the germ cell, ensuring a more thorough kill.
That said, 90%+ alcohol still has its place—especially when it comes to electronics. Moisture and circuitry are a bad mix, so using a higher percentage alcohol means quicker evaporation, reducing the risk of water damage while still providing decent cleaning power.
9. The Truth About Organ Transplants: What Happens After the Happy Ending

In movies, getting an organ transplant is the emotional climax—the part where the beeping slows, the surgery is a success, and everyone breathes a sigh of relief. Fade to black, roll credits. But in real life? That’s just where the next chapter begins—and it’s not always a smooth one.
While receiving a transplanted organ can indeed be life-saving, the idea that everything is “fixed” afterward is a huge misconception. Even with the best donor-recipient match, your body still sees the new organ as a foreign invader. That means your immune system is going to try to destroy it.
To keep that from happening, transplant patients must take immunosuppressive drugs—for life. These medications are powerful and necessary, but they come with a hefty list of side effects. For instance, the very drugs that prevent rejection also leave your immune system compromised, making you more vulnerable to infections.
And there’s more: a not-so-rare condition called post-transplant diabetes mellitus can develop, often triggered by the long-term use of steroids and anti-rejection meds. This form of diabetes adds another layer of complexity to a life that already requires constant medical supervision.
8. The Flu Vaccine: Separating Facts from Myths
It’s an undeniable reality that each year, a significantly smaller number of people roll up their sleeves for the flu shot compared to those who dutifully get their regular booster shots and other vaccinations. There are various reasons people give for dodging the flu vaccine, and some of these reasons are more misguided than others.
Some folks claim that the flu shot is mainly for older adults, young children, or individuals with compromised immune systems. They seem to think that their own immune systems are strong enough to fend off the flu without any external help. They even go as far as to say that they could handle a minor case of the flu without much trouble. In fact, they believe that getting the flu shot might actually give them a mild case of the flu, so they’d rather avoid the perceived risk altogether. Others argue that the flu shot is largely ineffective, a waste of time and effort, and that it seldom does what it’s supposed to do.
However, the truth is that most of these excuses hold no water. First and foremost, it’s a complete fallacy that you can catch the flu, even a mild version of it, from the flu vaccine. The components of the flu virus included in the vaccine are inactivated, meaning they’re dead and incapable of coming back to life, let alone causing an infection.
It’s true that some people may experience a few mild symptoms that are commonly associated with the flu after getting the vaccine. These symptoms are typically short – lived, lasting only a few hours or days at most. This can cause some confusion, as people might wrongly assume that they’ve actually contracted the flu from the vaccine. But rest assured, these symptoms are just a normal immune response to the vaccine, not a sign of an actual flu infection.
Now, let’s address the other misconceptions one by one. The flu shot is not just for the elderly, young children, or those with weakened immune systems. In fact, everyone aged six months and older should consider getting the flu shot. The flu can have a significant impact on workplace productivity, causing a lot of lost workdays. The collective cost of this lost productivity far outweighs any potential side effects that might occur from the vaccine.
Moreover, just because the flu shot doesn’t always work doesn’t mean it’s ineffective. Each year, scientists carefully analyze the flu strains that are expected to be the biggest culprits during the upcoming flu season. They then develop the vaccine with the specific goal of targeting these strains. So, while the flu virus is a cunning and adaptable foe, the flu vaccine is our best line of defense against it.
7. The Myth of Sucking Venom Out: Why It’s Not the Miracle Cure in Real Life

In countless movies and tales—from the enigmatic cases of Sherlock Holmes to age-old legends—the idea of sucking venom from a wound has captivated audiences. It’s a classic trope: a desperate attempt to stave off the lethal effects of a venomous bite by manually drawing out the poison.
But here’s the reality check: while it may seem like a smart move in the midst of a crisis, the truth is far less cinematic. Even though there have been extractor devices designed to pull venom from wounds, extensive scientific studies have shown that they are ineffective in preventing venom from spreading through the bloodstream.
In actuality, venom from most creatures spreads more slowly than movies would have you believe. The priority in a venomous bite situation isn’t to try and suck the toxin out, but rather to get the victim to a hospital immediately for the proper antivenom treatment. Attempting to extract the venom manually not only fails to remove it faster than the body’s own circulation, but it can also be hazardous—imagine accidentally poisoning yourself if there’s an open wound in your mouth!
The enduring appeal of this trope in literature and film might explain why some still swear by its use, despite the grim and scientifically backed advice that it simply won’t work. Modern medical consensus is clear: prompt professional care is your best bet against venomous bites, not home remedies or cinematic antics.
For more insights on venom management and first aid, you might visit the CDC’s guidance on snake bites or explore WHO’s recommendations on managing envenomation.
6. No, You Shouldn’t Stab Someone’s Heart With Adrenaline for an Opioid Overdose

That unforgettable moment in Pulp Fiction—you know the one—where John Travolta plunges a giant needle of adrenaline straight into Uma Thurman’s heart? It’s burned into pop culture memory. It’s dramatic, it’s wild, and… it’s almost entirely medically inaccurate.
While the scene makes for great cinema, in the real world, stabbing adrenaline (epinephrine) into someone’s heart isn’t just unnecessary—it’s dangerous. The method shown is known as an intracardiac injection, and it’s almost never used outside of extremely rare emergency situations—and even then, only by trained medical professionals, slowly and precisely, not with the chaotic flair of a Tarantino character.
What makes this even more misleading? Uma Thurman’s character is overdosing on opioids, not going into cardiac arrest from an allergic reaction or other shock-related issue where adrenaline might be indicated. In cases of opioid overdose, adrenaline won’t help at all.
What you actually need is Naloxone, commonly known by the brand name Narcan. This life-saving medication is designed specifically to reverse the effects of opioid overdoses. The good news? It’s often administered as a nasal spray, making it accessible even to non-medical responders. And if the person isn’t breathing, your next move should be CPR, not grabbing a needle.
5. Glasses Can’t Fix Everything: The Surprising Truth About Vision Problems
Most people think of glasses as magical tools—like modern-day goggles that turn blurry worlds crisp again. And for many, they really do. You put them on, and boom—suddenly you can read street signs, see people’s faces, or stop squinting at your phone. But here’s something most people don’t realize: glasses are not a cure-all. In fact, for some people, glasses don’t help much at all.
We live in a world where vision issues are incredibly common. If you don’t wear glasses yourself, chances are you know someone who does. But the assumption that everyone with poor vision can just “get glasses” and see clearly is a big misunderstanding. Some conditions go way beyond what corrective lenses can help with. And that’s where it gets both fascinating and a little heartbreaking.
Take legal blindness, for example. It doesn’t mean someone is completely blind. Instead, it refers to a very specific measurement: a person is legally blind if what they see at 20 feet is what someone with normal vision can see at 200 feet. So yes, they may still see shapes, colors, or movement—but glasses can’t always sharpen that image.
Then there are eye diseases that don’t respond to any kind of lens correction. These include macular degeneration (which affects central vision), diabetic retinopathy (a complication of diabetes that can lead to blindness), and optic nerve damage. Even prolonged exposure to sunlight can damage parts of the eye in ways no prescription can fix.
And while science is always making progress—there are experimental treatments, high-tech implants, even gene therapy in the works—the reality for many people is that those options are years away, expensive, or still too risky.
4. “Feed a Cold, Starve a Fever”? Not So Fast — Here’s What Science Really Says

You’ve probably heard the old saying: “Feed a cold, starve a fever.” It sounds wise, almost mystical—like something passed down by your great-grandmother alongside secret soup recipes and home remedies involving garlic and ginger. And believe it or not, this phrase dates back to at least 1574, when it appeared in a dictionary compiled by John Withals.
For centuries, this catchy line stuck around. Parents repeated it. Teachers nodded at it. Even some health-conscious folks still swear by it today. The idea seems logical, right? Colds and fevers must work differently in the body, so maybe they require opposite strategies?
But here’s where things get curiously off track.
There is zero scientific evidence—yes, zero—supporting the idea that you should withhold food from someone with a fever. In fact, the human body is incredibly demanding when it’s sick. Whether you’re fighting off a cold, the flu, or just battling a mild fever, your body is working overtime to push out invaders. That means it needs fuel—in the form of calories, fluids, and rest—to mount an effective defense.
Let’s break it down. A cold is usually caused by a virus, not bacteria, and so is the flu. Both trigger an immune response that raises your body’s temperature. A fever isn’t the enemy—it’s a sign your system is firing on all cylinders. And that takes energy. Starving the body during this time doesn’t “burn out the illness”; instead, it can weaken your immune response, slow recovery, and make you feel worse overall.
3. Think Calling an Ambulance Gets You Seen Faster? Think Again

Have you ever heard the belief that if you call an ambulance, you’ll be seen at the hospital faster? It’s one of those ideas that’s been passed around so much, it seems like common sense to some. After all, ambulances race through traffic, right? Surely, that means you’ll get seen quicker if you show up in one, right?
While this might sound logical in the heat of the moment, the reality is quite different, and it’s an important misconception to clear up.
The truth is, ambulances are designed for a very specific purpose: to transport people who are in need of urgent medical care or who can’t get to the hospital by any other means. They aren’t a VIP pass to the front of the line. When you arrive at the hospital—whether by ambulance, taxi, or even walking through the door yourself—you’ll be treated based on the severity of your condition. This system is called triage, and it ensures that the most critical patients are prioritized.
So, here’s where things get interesting: calling an ambulance when you don’t need it can actually create problems. It ties up valuable resources, from paramedics to hospital staff, that could be better used on someone who truly needs immediate attention. In fact, ambulance services are under significant pressure as it is. Using them for non-urgent situations only makes it harder for those in real emergency situations to get the help they need quickly.
If you can safely make it to the hospital by other means, and you’re sure you can get there in time, skip the ambulance. It won’t get you seen faster, and it might even delay care for others.
2. Defibrillators: Not Magic Heart Restarting Paddles, But They’re Still Amazing
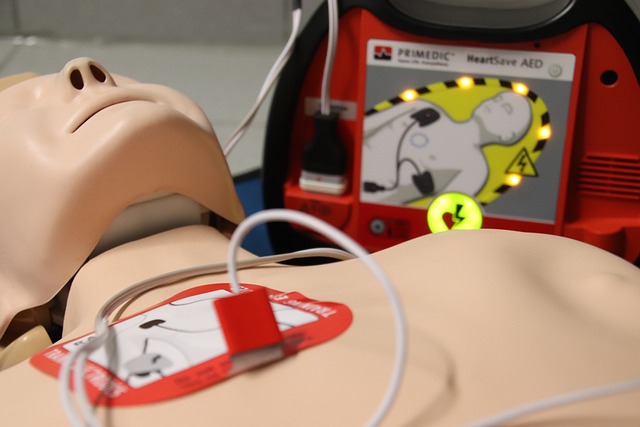
If you’ve ever watched a medical drama, you’ve seen the scene countless times: the defibrillator paddles are charged, the doctor dramatically yells “Clear!” and the electricity zaps through the patient’s chest. Within moments, the person miraculously wakes up, gasping for air. It’s tense, it’s thrilling, and for many, it’s the moment that defines the show. But what if I told you that defibrillators aren’t exactly the magic heart-restarting devices they’re made out to be?
As much as we love these high-stakes, heart-pounding scenes, the reality is a bit less dramatic. While defibrillators can save lives, they do not work like the ones in TV shows. The truth is, they don’t “restart” a heart that’s completely stopped. They’re designed to correct abnormal heart rhythms, like ventricular fibrillation or tachycardia—conditions where the heart is still technically beating, but in a chaotic, ineffective pattern. A defibrillator can deliver a shock that helps the heart reset into a normal rhythm.
A 2014 study of resuscitation scenes in movies and television uncovered how often these scenes got it wrong. They found that many of the scenes misrepresented the function of defibrillators, leading to a lot of confusion. Instead of saving the day with a dramatic zap, defibrillators are part of a more complex medical process—one that includes timely CPR, oxygen, and skilled care from medical professionals.
While they’re not as magical as TV shows would have us believe, defibrillators are still incredibly powerful tools when used correctly. They don’t bring someone back to life from a dead heart, but they can help someone’s heart rhythm stabilize and give them a better chance of survival.
1. The Truth About Seizures: Don’t Stick Anything in Their Mouth

Seizures are often a dramatic moment in TV shows, with people rushing to get something in the mouth of the person seizing, in an attempt to prevent them from biting their tongue off. This scenario has become so popular in medical dramas—like E.R. and House—that it’s easy to think this is the best thing to do in a real emergency. But here’s the truth: sticking something in the mouth of someone having a seizure is not only unnecessary, it can be dangerous.
Let’s clear up the biggest myth first: It’s impossible to bite off your tongue during a seizure. While it’s true that someone having a seizure may bite their tongue, they can’t actually sever it. What can happen, though, is that they can injure their tongue and cause painful cuts. This is where the misconception arises. So, instead of trying to prevent a non-existent “tongue-biting-off” scenario, there’s a far more important job at hand.
The priority during a seizure is to ensure the person’s airways remain clear. Avoid trying to stick anything in their mouth—this could block their breathing or cause injury. Instead, focus on keeping them safe: Move any nearby objects that they might hurt themselves on, timing the seizure, and calling for medical help if the seizure lasts longer than five minutes or if they have another seizure soon after.
In short, if you ever find yourself in a situation with someone having a seizure, don’t try to shove something in their mouth. Protect their surroundings, keep their airways clear, and seek professional medical assistance when necessary.